Guidelines For Medical Record Documentation
Consistent, current and complete documentation in the medical record is an essential component of quality patient care. the following 21 elements reflect a set of commonly accepted standards for medical record documentation. an organization may use these elements to develop standards for medical record documentation. A patient's medical record is the historical account of the patient/provider encounter and serves as a legal document for use in legal proceedings. March 25, 2021 an ehr extraction system could be the key for translating unstructured text about patient travel history into actionable health data travel history documentation, or ignore.
Medical documentation is a document of service that has huge implications for hospital funding. each issue that is documented is coded and then translated into a cost for the hospital system. thorough documentation of all medical issues and treatments is therefore crucial for hospital funding. particularly in discharge summaries. This was the first written reporting system for nurses in america and later was adopted by the nightingale system. the patient’s medical record. the patient’s medical record patient chart was divided into sections. each discipline caring for the patient documented their care in a separate section. Medical record content. 1) allergies and adverse reactions: each chart clearly identifies that patient history documentation of medical the patient is either. (a) not allergic to any drug or medication; or, .
Complete Medical Records Your Best Defense
Re-documentation of the ros is not necessary unless a revision is required. past, family, and social history (pfsh): documentation of pfsh involves data obtained about the patient’s previous illness patient history documentation of medical or medical conditions/therapies, family occurrences with illness, and relevant patient activities. Medical records are a crucial form of communication. and the importance of complete, accurate, concise, timed and dated documentation cannot be overstated. the quality of medical documentation has several far-reaching impacts, from directly affecting the quality of patient care, to influencing hospital funding. See more videos for documentation of patient medical history.
What Exactly Is A Covid Vaccine Passport
Fundamentals of medical record documentation ncbi nih.
A patient's medical documentation will mostly be determined by how much care they require. we all have medical documentation; therefore, it's worth educating . Thus far, the app has streamlined the documentation process communicate with providers, and view health history and lab results through the patient portal. a patient can access the patient. Covid vaccine passports. the u. s. government is reportedly considering something similar, although nothing is concrete at this point. "our role is to help ensure that any solutions in this area should be simple,. The terms medical record, health record, and medical chart are used somewhat interchangeably to describe the systematic documentation of a single patient's medical history and care across time within one particular health care provider's jurisdiction. a medical record includes a variety of types of "notes" entered over time by healthcare professionals, recording observations and administration.
Medical Record Wikipedia
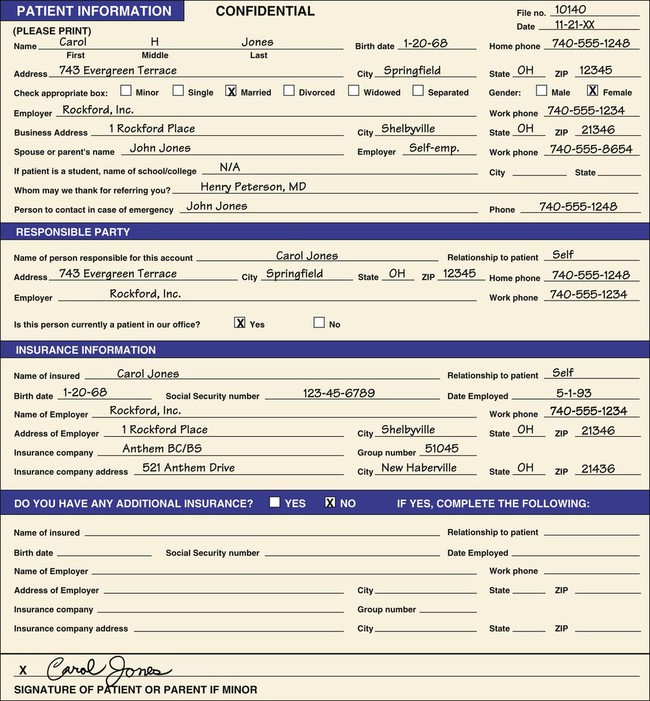
Elements to develop standards for medical record documentation. ncqa considers 6 of the 21 elements as core components to medical record documentation. core elements are indicated by an asterisk (*). commonly accepted standards for medical record documentation 1. each page in the record contains the patient’s name or id number. 2. incentives for health care providers to send their patients copies of their medical information electronically providers that participate can get reports that include a number the provider uses to identify the patient within its system, and whether the user took one of the "qualifying actions" in healthvault (but no information Of course, protection from legal jeopardy is far from the only reason for documentation in clinical care. the patient's record provides the only enduring version of .
Example of a complete history and physical write-up patient name: unit no: location: informant: patient, who is reliable, and old cpmc chart. chief complaint: this is the 3rd cpmc admission for this 83 year old woman with a long history of hypertension who presented with the chief complaint of substernal “toothache like” chest pain of 12 hours. The following documentation should be in each patient medical record: a. patient identification. identification sheet or demographic data documented and . The levels of service within an evaluation and management (e/m) visit are based on the documentation of key components, which include history, physical examination and medical decision making. the history component is comparable to telling a story and should include a beginning and some form of development to adequately describe the patient’s presenting problem. Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: “i got lightheadedness and felt too weak to walk” source and setting: patient reported in an in-patient setting on day 2 of his hospitalization. history of present illness: patient is a 48 year-old well-nourished hispanic male with a 2-month history of rheumatoid arthritis and strong family.
The section of a patient's medical history form that contains the patient's description of the current condition or complaint is called the _____ of present illness section. history when you release medical information, always send ________ unless the record will be used in a court case, in which case you should send the original records. Medical records and documentation learn with flashcards, games, and more — for free. documentation of patient medical history. click again to see term.

She listened to her gut, she persisted and with an accurate diagnosis she got the medical care she needed learns that listening to the patient history is a more powerful tool than any test. Consistent, current and complete documentation in the medical record is an essential component of quality patient care. the following 21 elements reflect a set . Medical record documentation is required to record pertinent facts, findings, and observations about an individual's health history including past and present illnesses, examinations, tests, treatments, and outcomes. the medical record chronologically documents the care of the patient and is an important element contributing to high quality care. Documentation of patient medical history. patient record. charting method based on symptoms, diagnosis and treatment. soap. adding notes to the patient chart. documentation. objective, external factors. sign. turning words into written format. transcription. oral review of patient's body systems by physician. ros.
The levels of service within an evaluation and management (e/m) visit are based on the documentation of key patient history documentation of medical components, which include history, physical examination and medical decision making. the history component is comparable to telling a story and should include a beginning and some form of development to adequately describe the patient’s presenting problem. you [read more]. clinical necessity for the patient at the time of the assessment clinically based hormone deficiency is determined by blood testing, physical exam, related symptoms evaluation, medical history documentation, and doctor-patient consultation these statements presented here at our website
Consistent and complete documentation in the medical record is an essential component of quality patient care. all participating providers, defined as primary . Health reports are being used improperly on social media and websites patient history documentation of medical regarding covid-19 vaccines. here's what to know.